Meet the new pox; same as the old pox
Pictorial Press Ltd/Alamy Stock Photo
The U.S. response to the COVID-19 pandemic was far from ideal. Let’s stipulate to that. From the fumbled initial testing effort to former President Trump’s habitual misinformation about the disease and its treatments to the slow rollout of vaccines, the U.S. stumbled every step of the way.
Inequities abounded in infection and mortality rates, treatment, and vaccination. Hispanic, Black, and Native Americans were disproportionately likely to become infected with (and die from) COVID-19. And when science delivered vaccines in record time, they were snapped up by high-income countries, restricting access for low- and middle-income countries. Within the U.S., with the notable exception of prisoners, we initially allocated vaccines according to risk status. But on a global scale, they were distributed mostly in relation to economic power and contractual agreements that largely slammed the door on developing countries, particularly in Africa.
To avoid this predictable injustice, the COVAX initiative was started early in the pandemic by the World Health Organization (WHO) in partnership with the Coalition for Epidemic Preparedness Innovations, Global Alliance for Vaccines and Immunization (Gavi, the Vaccine Alliance), and the United Nations Children’s Fund. Its goal was to enable “access to potential COVID-19 vaccines to the most vulnerable everywhere, regardless of income level.”
COVAX vaccine doses started shipping in February 2021 and the group has since distributed over 1.7 billion doses to 146 countries. Yet, compared to other regions (Latin America, U.S. and Canada, Asia-Pacific, Europe, and the Middle East) where between 58% and 82% have received at least one vaccine dose, Africa’s vaccination rate languishes at 30%. In African countries like Madagascar, Cameroon, and Senegal, less than 10% of the population has received a single dose.
With all that experience so recently under our belt, you’d think the planet would be better equipped for the next outbreak. In future global health emergencies, the world’s actions would be anchored in “equity, solidarity, and responsiveness,” at least according to a strategic document presented at a September 2021 session of the WHO Regional Committee for Europe. Surely, we wouldn’t make the same mistakes.
Think again.
The U.S. was hit with its first case of monkeypox (MPox) in May 2022 and, two months later, the WHO declared the MPox outbreak a public health emergency of international concern. MPox has been endemic for years in 10 countries in Africa. There, a milder strain is found in West Africa while a more lethal strain exists in the Democratic Republic of the Congo (DRC) and the Central African Republic. Very little international attention has been paid to this endemic disease despite thousands of suspected cases in the past decade in the DRC alone (this is likely an undercount because of limited testing and surveillance). It took the spread to wealthier nations for the rest of the world to sit up and pay attention.
It’s not as if the U.S. MPox response has been ideal, but we actually began with a head start. Unlike in the early days of COVID-19, viable vaccines were available for MPox in the form of smallpox vaccines. (In the 1980s, a small study suggested that smallpox vaccines would protect against MPox.)
When smallpox was eradicated in 1980, global smallpox vaccination ceased, though the WHO and a handful of countries, including the U.S., keep vaccine stockpiles in case the virus is accidentally unleashed from labs or used as a bioweapon.
In addition to its large stockpile of original smallpox vaccines, the U.S. in 2007 awarded a contract of almost $550 million to the Danish vaccine company Bavarian Nordic for 20 million doses of its new smallpox vaccine – now called Jynneos – that was easier to administer and safer than earlier vaccines.
The U.S. continued purchasing the vaccine in subsequent years and in 2019 it was approved by the Food and Drug Administration for the prevention of smallpox and monkeypox. But by then, all of the nearly 30 million doses of Jynneos in the U.S. stockpile had expired. Yes, you read that right. Even as people in Africa continued to suffer and die from MPox, the U.S. let its stockpile of new vaccines expire.
The scramble for vaccines following the spread of MPox to high-income countries in May 2022 zeroed in on Bavarian Nordic’s vaccine. The company had 16 million doses on hand, of which about 15 million were claimed by the U.S. The remaining doses were quickly purchased by Canada, Australia, and European countries. Nothing for Africa. Sound familiar?
However, the limited supply is not the only factor hampering access to vaccines. The price of Jynneos is $110 per dose for any buyer, with discounts only for high-volume purchasers. This price is prohibitive for lower-income countries. Though the Latin American arm of the WHO has obtained a small donation of vaccines for that region, the WHO has yet to provide guidance on getting vaccines to all the countries in need. Right now, most of the over 100 countries reporting MPox cases have no available vaccine, not to mention shortages in tests and treatments.
This tragedy could have been avoided if, in addition to a more equitable vaccine distribution, investments had been made earlier into researching ways to identify, prevent, and treat MPox infections. But there was little interest in such investments when the disease was confined to countries in West and Central Africa. MPox has proved to be yet another “disease of the poor” that fails to draw attention until it affects wealthy countries. And these western world practices have assured that the vaccines have not saved nearly the number of lives they could have.
COVID-19 and MPox may both be caused by viruses, but the biological similarity ends there. Compared to COVID-19, MPox is not as easily transmitted, is less likely to evade immunity from vaccines because it is a DNA rather than RNA virus, and its fatality rate is much lower.
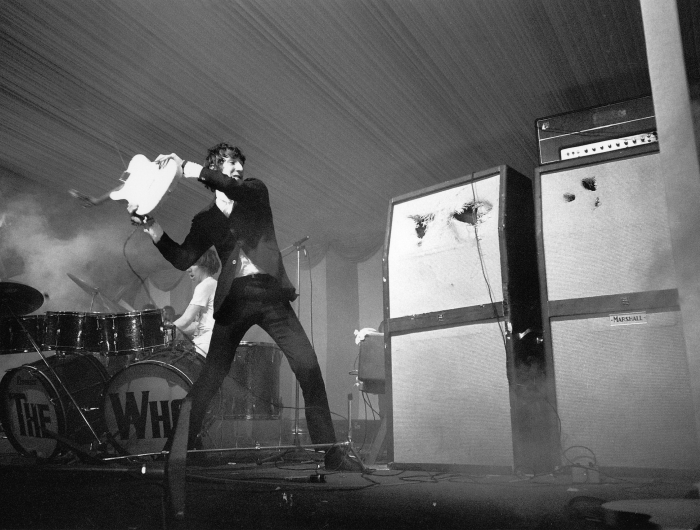
But the two diseases share the anemic nature of the global response to each. It is that response that is the true pox: an affliction of indifference, elitism, and racism that seems to characterize our every response to public health emergencies. In that sense, with apologies to The Who’s Pete Townsend, we have been infected by the same old pox. What will it take so that we “Won’t Get Fooled Again”?
Tags
Topics

