Separating gluten-free fact from fiction

Stomach pain, diarrhea, weight loss. Those are some of the symptoms of celiac disease, which is an autoimmune reaction to gluten, a protein found in wheat, barley, and rye. At least one out of 100 Americans have celiac. Most of them don’t know it. And studies suggest that some people who don’t have the disease still can’t tolerate gluten.

Joseph Murray is a gastroenterologist and professor of medicine at the Mayo Clinic in Rochester, Minnesota. He is a senior associate editor of the American Journal of Gastroenterolgy and the author of a study on the rising incidence of celiac disease. Murray spoke to Nutrition Action's Bonnie Liebman.
What is celiac disease and how common is it
Q: Is the incidence of celiac rising?
A: Yes. It has increased dramatically in the U.S. since 1950, and now affects 1 percent of the population. There’s good evidence that we’re not just getting better at detecting celiac. It’s also increasing in other countries, even in places where it was historically common, like Finland. And celiac disease occurs at every age. It occurs out of the blue in elderly people as well as in children.
Q: Why is celiac increasing?
A: There are many theories. For example, something may have changed in the way we grow, process, and eat wheat that may have affected our likelihood of getting celiac disease.
There is a drive to provide higher-gluten wheat because that’s what makes bread springy and makes a good sliced loaf. And the ongoing breeding to generate new strains that are disease resistant or higher yield—that’s a prime suspect.
Q: What causes celiac disease?
A: If you have a genetic predisposition, your T cells—T lymphocytes—start to see gluten as an enemy. Think of your body’s immune system as the FBI. Once it sees gluten as an enemy, it sets up what we call a memory response.
It’s like the TSA watch list for people who fly. Once you’re on it, it’s very hard to get off. Once you’re tagged by the immune system, you’re tagged forever. You can go off gluten for a year, and your intestine can heal, but once it gets gluten back, bam, here it comes again.
Q: How does gluten become an enemy?
A: The gluten probably gets changed by one of our human enzymes called tTG, or tissue transglutaminase, so it becomes more antigenic—that is, it looks more like a foreign invader. Then the T cells get hold of it, and they traffic it to the draining lymph nodes and set up an aggressive immune response.
Q: And something triggers the response?
A: Yes. Thirty percent of the population carries one of two versions of the gene for the disease—HLA DQ2 or DQ8—and essentially everybody eats gluten, yet most of us don’t get celiac. So something triggers it—infection, injury to the intestine, surgery, drugs, or something else.
Q: How does celiac harm the intestine?
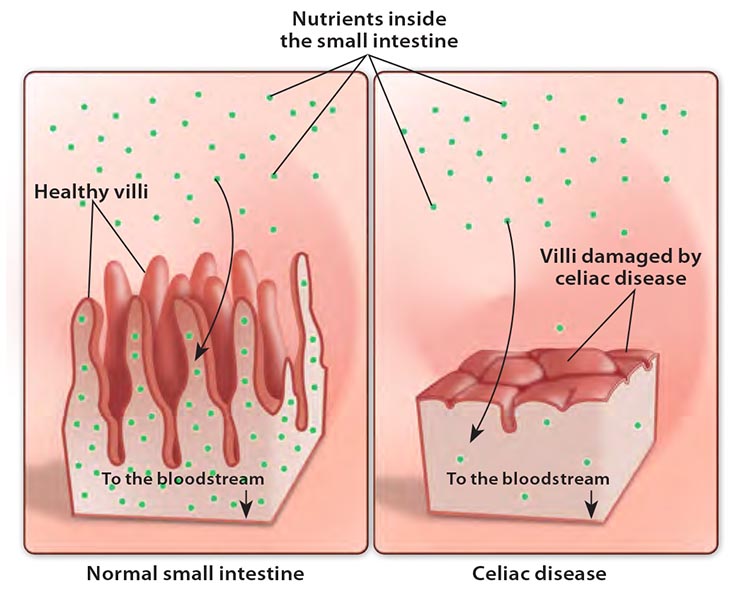
A: If you have celiac disease and you keep eating gluten, the damage accelerates and you get chronic inflammation. And the body produces cytokines, or chemical messengers, from the inflammation that make people feel crummy. They may not even point to their gut, which is where the problem is coming from. They just say, “I feel terrible.”
The inflammation starts to recruit other players, and soon you’ve got a ruckus going on in the intestine. Eventually, it damages the lining of the intestine and your ability to absorb nutrients.
Q: Is it true that most people with celiac have no GI symptoms?
A: Probably. And most people who have celiac disease don’t know it. Some don’t know it because they don’t have symptoms. Other people go to the doctor with anemia or other problems, but celiac disease is not suspected so they’re not tested for it.
But here’s the kicker. Let’s say you look at people you found by doing a screening. You ask if they’ve got any symptoms and they say, “No Doc, I feel fine. My digestion is perfect.” Then you put them on a gluten-free diet, and when you see them a year later they say, “My bowel habit is much better than it was.” You say, “Huh? But I thought you said you had no symptoms.” What they’d accepted as normal, they now know wasn’t. That’s pretty common.
Q: Do some people without celiac disease react to gluten?
A: Yes. In 1980, researchers in England fed women with chronic diarrhea a gluten- free diet or not. And their symptoms went away on the gluten-free diet. It’s not quite celiac disease, but patients have the celiac genes. They may or may not have the antibodies. They may just have slight damage in the intestine. I would call that celiac lite.
Q: They have a mild version of celiac?
A: Yes. There’s also a celiac-like condition. We call it non-celiac gluten intolerance. There’s a lot of debate about it. Patients have symptoms that look like celiac disease or irritable bowel syndrome, and they get better when they go on a gluten-free diet. But they don’t necessarily have the genes for celiac disease. And they don’t have antibodies for celiac.
In a very good recent study, an Australian group fed these people either a gluten-free diet or not in a double-blind, placebo-controlled fashion. Those who were fed gluten got their symptoms back.
You can think of it as gluten-sensitive irritable bowel syndrome because it’s like IBS, but the symptoms get better when people go on a gluten-free diet.
Gluten-free diets
Q: Do some people feel better on a gluten-free diet just because they expect to?
A: Yes, there is a strong placebo response. It could last a few months. Then they could get fed up with it.
When people talk about feeling better when they go gluten free, any of ten different things could probably explain it.
In some people, it could be that when they eat less gluten, they eat less food. Eating less is the most important advice we can give to most Americans. Or they may feel better just because they eat less junk food. If you get rid of the gluten, it’s harder to eat junk.
Q: Aren’t some gluten-free foods also junk?
A: There are plenty of gluten-free foods that are unhealthy for you. And there have been studies showing that a gluten-free diet may have less fiber and vitamins. Many gluten-free foods are not fortified, so that’s also an issue.
Testing for Celiac Disease
Q: Should everyone get tested for celiac?
A: The jury is out on that. Celiac disease is common, it’s got consequences, there’s a blood test you can do that will detect it fairly easily, and there’s a safe treatment—a gluten-free diet—that’s not easy to follow, but it’s safe.
But we’re not at the point of being able to prove that it’s cost-effective to screen everyone. And we don’t know if people, once identified, will actually go on a gluten-free diet.
Q: So who should be tested?
A: Anybody who has a family member with celiac disease or symptoms that are suggestive of celiac disease—like iron deficiency anemia, chronic diarrhea, bloating, gas, or abdominal pain. So should people with type 1 diabetes or autoimmune diseases like lupus or rheumatoid arthritis in the family.
Think of all the ways that celiac disease can make itself known—chronic fatigue, infertility, a skin rash called dermatitis herpetiformis, or nervous system problems like nerve damage or a loss of muscle coordination called ataxia.
It can also show up as bone problems like premature osteoporosis or osteomalacia, which is a softening of the bones due to lack of vitamin D, or as severe joint problems called arthralgias.
Doctors may not think about celiac disease because these are common problems, and other explanations for them are probably more likely than celiac.
Q: How do you test for celiac?
A: A blood test for antibodies to tissue transglutaminase is the first step. If the tTG test is positive, the current recommendation by virtually every organization is to get a biopsy of the lining of the small intestine.
Q: Why do you need a biopsy?
A: If the tTG test is positive, that increases your probability of having the disease ten-fold. So if somebody has terrible diarrhea or they’re anemic and has a brother with celiac, their likelihood of having the disease is one in two. If their tTG test is positive, it’s virtually certain that they have the disease.
On the other hand, if a patient comes to me and says, “I’ve got chronic fatigue, Doc. And I’ve got a bit of bloating.” Well, the chances that they have celiac disease if they have no family history are probably about 1 in 30. A positive tTG test increases the likelihood ten-fold, so the patient’s chance of having celiac disease is one in three. That means two out of three patients with a positive test won’t have the disease.
That’s not a solid basis to make a diagnosis and put someone on a diet. You’ve got to biopsy them.
Q: Is a biopsy definitive?
A: Yes, as long as the patient isn’t already on a gluten-free diet. If they are, the biopsy may not see signs of celiac. The same is true for the blood test. That’s all the more reason that people should get tested before going on a gluten-free diet.
Q: What if the tTG test is negative?
A: A negative tTG test reduces their chance of having celiac ten-fold. So it goes from one in 30 to one in 300. That’s pretty darn low.
Q: What’s the harm in not getting tested?
A: If people derive some benefit from a gluten-free diet without getting tested, I would never argue with success. But there are risks.
People could have other diseases like Crohn’s disease, peptic ulcer disease, or colon cancer. Those conditions could go untreated while the patient focuses on avoiding gluten. So before people go on a diet like this, they need to know what they have or don’t have.
Q: Should doctors test people who have irritable bowel syndrome for celiac disease?
A: Yes. And if no alternative diagnosis suggests itself to me, I will say, “You could try a gluten-free diet.”
Q: Is it good that gluten-free foods are showing up everywhere?
A: Yes, because that makes it a lot easier for people with celiac. The danger with that trend, though, is that it may trivialize a real disease. So while we think, “Oh, everyone is on a gluten-free diet. It’s no big deal,” it is a really big deal for people with celiac, and it’s a super big deal for people with severe complications including lymphomas, carcinoma of the small intestine, and maybe esophageal cancer.
Q: Are those cancers going up because celiac is more common?
A: No. How much of the risk of lymphoma is due to celiac? Tiny. Super duper tiny. How much of the risk of lung cancer is caused by smoking? Now that’s a high number.
llustration: Timothy Cook/NIH Medical Arts, Jorge Bach/CSPI.

