Are COVID-19 racial disparities really a thing of the past?

CDC.
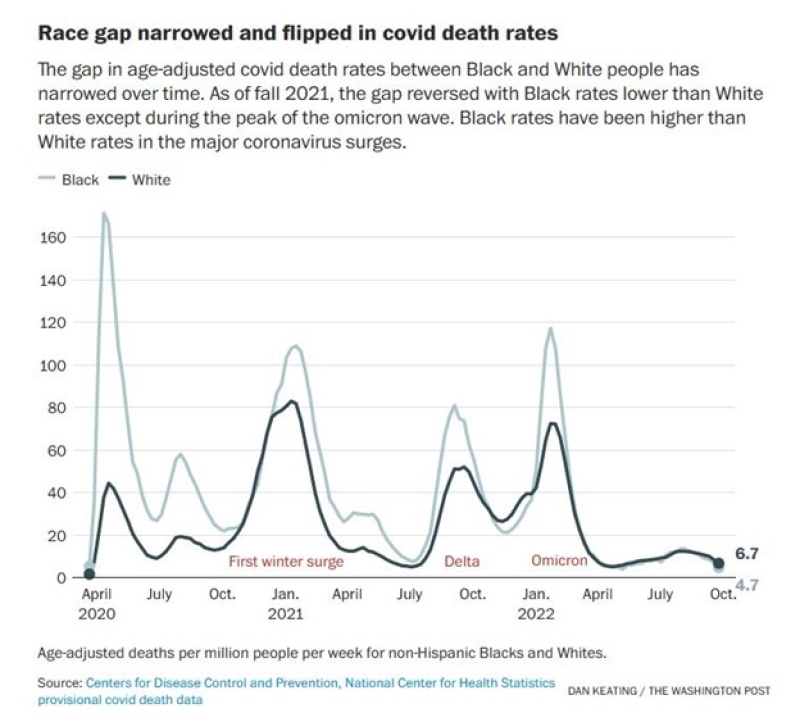
“Whites now more likely to die from covid than Blacks,” announced the Washington Post headline in October above an article analyzing COVID-19 mortality rates during the pandemic.
If true, that’s quite a reversal. Early in the pandemic, deaths were concentrated in dense urban areas, where Black people died at three or more times the rate of White people.
We have a pretty good idea why this happened. People who worked closely with the public in service jobs and couldn’t stay home to telecommute, who lacked sick leave and adequate health insurance, lived in multi-generational housing, were employed in workplaces without adequate workplace protections, or depended on public transportation were more likely to contract COVID-19.
Similarly, those who may not have had access to quality medical care, have underlying health conditions, or faced discrimination or language barriers in the healthcare systemwere more likely to die from COVID-19 infections.
These hurdles haven’t changed very much, if at all, as we discussed in a previous blog. Among adults treated for COVID-19 infection from January to July last year, White patients were approximately twice as likely to be treated with the antiviral drug Paxlovid as were Black or Hispanic patients, based on a survey of 30 U.S. healthcare systems.
According to the Post’s analysis of CDC data, the large mortality gap between the races early on has narrowed over time until nearly two years into the pandemic, in the fall of 2021, the mortality rate for White people for the first time exceeded that of Black people.
This slightly greater mortality rate of White people has persisted since then, except during the peak of the Omicron variant wave a year ago when Black people once again were considerably more likely to succumb to COVID-19. But after the Omicron wave receded, White people reverted to being slightly more likely to die from COVID-19.
Do these trends represent a triumph for fairness and an end to COVID-19 racial disparities?
Not really.
The overall mortality rates of Black and Latine people from COVID-19 since the beginning of the pandemic remains far greater than the mortality rate for White people and will almost certainly stay that way over the course of the pandemic.
Through the end of 2022, the COVID-19 mortality rate for Black people was 1.6 times and for Latin people 1.7 times that of White people.
This awful disparity in COVID-19 deaths is reflected in the dramatic and asymmetrical decline in life expectancy at birth in the United States between 2019 and 2021. It fell 6.6 years for Indigenous people, 4.2 years for Latin people, and 4.0 years for Black people, compared with 2.4 years for White people and 2.1 years for Asian Americans, according to CDC data.
New research published in November looking at what occurred during the pandemic in Ohio and Florida suggests a possible explanation for why White people have become slightly more likely to die from COVID-19 than Black people.
Yale University researchers compared the overall mortality rates in the two states before and then during the pandemic and found it was about 10 percent higher than expected during the pandemic years of 2020 and 2021. This is not surprising. Most of these “excess” deaths in 2020-2021 were likely due to COVID-19 infections, though some were presumably due to the ongoing opioid epidemic.
The Yale researchers then went further in their analysis. They had chosen Ohio and Florida because these are the only two states where they could link death certificates to voter registrations by name. With these data, they were able to determine whether voters registered as Republicans or as Democrats were more likely to succumb to COVID.
During the first year and a half of the pandemic, Republican and Democratic voters in the two states were equally likely to be among the pandemic’s “excess” deaths. However, this changed dramatically in the summer of 2021 when the mortality rate of Republican voters suddenly became nearly twice that of Democratic voters and then rose to about three times higher during the winter of 2021-22.
What happened? Well, it’s about the same time that vaccines became widely available to anyone who wanted one, the researchers pointed out. And we know that the vaccines are highly effective in preventing deaths from COVID-19.
Although the researchers couldn’t prove it from their data, the well-documented vaccine hesitancy among Republican voters could explain why they became more likely than presumably more-vaccinated Democratic voters to die of COVID-19 in these two states. (This research is consistent with other studies finding that the COVID-19 mortality rate was highest in the most Republican-voting counties in the United States.)
The uptick in Republican deaths from COVID-19 in Ohio and Florida, where White voters are much more likely to be registered as Republicans and Black voters much more likely to be registered as Democrats, happened at about the same time around the country that the national COVID-19 mortality rate for White people began to rise relative to Black mortality, according to the Washington Post analysis.
Another reason not to go overboard celebrating the current narrow racial difference in COVID-19 mortality rates is that it may be only temporary.
The social and economic conditions that contributed to the large mortality gap between White and Black people during the first half of the pandemic are largely unchanged and could manifest again if a new COVID-19 variant appears. Indeed, that is what the Post’s data suggest. Black and White mortality rates are similar when the pandemic curve is at its nadir, but when surges occur, as with the emergence of the Delta and the Omicron variants, the racial disparities reappear and Black people are more likely to suffer.
It is far too soon to declare victory over racial disparities in this pandemic. COVID-19 has been an unmitigated disaster for people with minoritized racial and/or ethnic identities, and the disparities in who perishes from it may well return with the next surge. Far better to identify the causes of these disparities and address them now, before the next pandemic.
Tags
Topics

